Enteropathic Arthritis
Enteropathic arthritis is a form of chronic, inflammatory arthritis associated with the occurrence of an inflammatory bowel disease (IBD), the two best-known types of which are ulcerative colitis and Crohn’s disease. About one in five people with Crohn’s or ulcerative colitis will develop enteropathic arthritis.
The most common areas affected by enteropathic arthritis are inflammation of the peripheral (limb) joints, as well as the abdominal pain and possibly bloody diarrhea associated with the IBD component of the disease. In some cases, the entire spine can become involved as well.
Is There a Cure?
Currently, there is no known cure for enteropathic arthritis but medications and therapies are available to manage the symptoms of both the arthritis and bowel components of the disease.
Causes of Enteropathic Arthritis
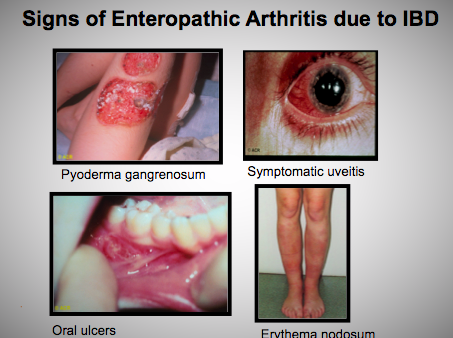
Many people don’t realize that the gastrointestinal tract contains the largest immune system in the body. The immune system is the body’s natural defense against foreign invaders, and it is somehow altered in people who have these conditions. Some researchers believe that the long-lasting inflammation found in the intestines of people with IBD damages the bowel, which in turn may allow bacteria to enter the damaged bowel wall and circulate through the blood stream. The body’s reaction to these bacteria may cause other problems including inflammation in the joints and/or spine, skin sores and inflammation of the eyes. Currently this hypothesis is neither fully understood nor confirmed by rigorous scientific study.
Ankylosing spondylitis and related diseases tend to run in families, so there is a genetic factor involved as well. Those who test positive for the HLA-B27 genetic marker are much more likely to have spinal involvement with enteropathic arthritis than those who test negative.
Disease Course/Prognosis
The course and severity of enteropathic arthritis varies from person to person. The disease ‘flares’ – the times when the disease is most active and inflammation is occurring – tend to be self-limiting, often subsiding after 6 weeks, but reoccurrences are common. In some cases the arthritis may become chronic and destructive.